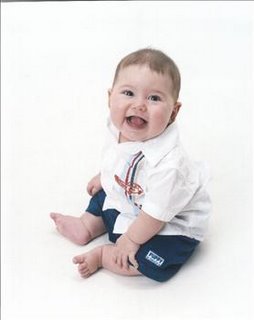
Hi! I’m Kaipo’i. Okay, it’s Kaipo’i Chace ‘Iolana-Clark. Oh geez, after today, I guess it’s Kaipo’i Chace Poliokekoa ‘Iolana-Clark. (I’ll have to thank my parents, grandma, and aunties later for tagging me with that one!) I want to thank you for spending this special occasion with me and my family. Wow! I’m a year old already. Seems like only yesterday that I was floating around in the womb oblivious to what lay ahead...
For those of you who may not know, I was born during a major celestial event. Last year the nine planets in our solar system were moving into the shape of an ellipse. This kind of thing doesn’t happen overnight. It took about a month for the planets to line up and another month for them to disperse. The culmination of this event was on May 6th, only 3 days after my birth. Just ask anyone who was working at the North Hawaii Community Hospital that weekend, and they’ll tell you it was a weekend for the record books. To begin with, I was born early Friday morning, May 3rd. My best friend Ryder Brown, was born the next day -- Saturday. On Sunday, there was another birth. Three babies with the same pediatrician and the same obstetrician all born with cardiac difficulties. The odds of all this is staggering. Fortunately, Ryder and I made it out of the hospital. Unfortunately, Sunday’s baby didn’t. (I hope it’ll be a very long time before the hospital staff or any families have to experience a weekend like that one. )
Needless to say, my birth was a major event. I was born at 4:10 a.m., and by 4:15 everyone knew there were problems. I was what used to be called a “blue baby.” Shortly after the doctor cut my cord, I started turning a remarkable shade of blue. By 6, I was on life support, and the NICU Transport Team was on it’s way from Kapiolani Women & Children’s Hospital in Honolulu. My Auntie Gail and Dr. Lee were there with us. They did the best they could to help my parents understand. My mom and dad were just beginning to learn how special I really was. They say they only remember bits and pieces of that morning. Mom says she understood words like “heart,” “Honolulu,” San Diego,” and “surgery,” but at that point they were just words, and they seemed to float around the hospital room unconnected and separate from her. My Dad says that he remembers the complete change of emotions. He stepped out of the room to call my big-big sister Kayla, and when he returned, he knew something was terribly wrong the minute he walked back in the door. His world, my world, our world had changed in minutes.
I was transported by helicopter to Oahu, and my parents and little-big sister Konane follwed me to Oahu that afternoon. (Mom had to be discharged from the hospital first!) They met with the doctors from the NICU at Kapiolani, and the medical terminology barrage began. Here’s what was made out in between: Holes in his heart. All internal organs not in “normal” location. Trying to make sure he has all his organs now. Has to be transported to San Diego immediately for surgery. Haven’t seen anything like him in over 10 years. Jet. Jet transport. It’s being scrambled out of Monterey right now. No. Only room for one parent to go. The others will have to stay here. Pack nothing bigger than a carry-on. We leave as soon as jet arrives. Nothing more we can do.
We arrived in San Diego at 5 in the morning (California time) on Sunday, May 5th. It was brutally cold and dark outside as they moved me from one isolette to another in order to transport me to the hospital by ambulance. My destination? Children’s Hospital & Health Center, NICU B. What we didn’t know was that this would be our home for the next month. We began with a barrage of invasive and non-invasive diagnostics in order to have a full understanding of just how special I really am. So, for those of you who have been waiting, here’s the whole shaboozie:
- Dextrocardia (my heart is on the right)
- Atrial Situs Inversus (the top 2 chambers of hy heart are reversed)
- Multiple Ventricular Septal Defects (there are large holes in the wall that divides the lower 2 chambers of my heart, so I basically am working with one big ventricle or bottom chamber)
- Double Outlet Right Ventricle (All my plumbing goes to the bottom right chamber only. Since it’s one big chamber anyway, this isn’t a problem. However, because everything is flowing to the right side, the left side isn’t being used or growing, so in November, we added Hypo-plastic Left Ventricle -- really small left chamber -- to the list too.)
- Pulmonary Atresia (the blood flow to my lungs is blocked. This is why I turned blue and the only condition they are correcting with surgery!)
- Abdominal Situs Inversus (all my internal organs are in opposite positions from where they are supposed to be – but they’re all there, and they all work just fine!)
- 2 left lungs (your right lung has three chambers for air– your left lung has two – that’s the design. I have two lungs that both have only 2 chambers. The doctors found this one really interesting when they discovered it during a Bronchoscopy.)
- Tracheobroncomalacia Right Lung (That means the main opening to my lung didn’t want to stay open on its own. This lung collapsed on me a few times, and it’s what kept me in the hospital much longer than originally anticipated, but it’s not a problem anymore.)
So after four days of every test possible, consultations, discussions among the cardiac team, discussions with members of the cardiac team, and telephone conversations between my mom and dad, the big consultation came. Mom met Dr. David Bichell, Director, Division of Cardiovascular Surgery at Children’s. The Big Kahuna. The Head Cheese. The Man himself was on the case. He was really nice and explained everything to my mom really well. He even drew pictures – most of the doctors did. Perhaps they drew them in order to help explain my unique design. Perhaps they drew them to see if they could. Perhaps a little of both. But Dr. Bichell drew an excellent picture and explained the Blalock-Taussig Shunt to my Mom. It was a routine procedure, and it would only be a temporary fix. It wouldn’t take more than 1 ½ hours. Knowing there wasn’t an option, Mom signed the consent and returned to her position–right by my side. I don’t remember the next day, but my Mom does. What was supposed to take 1-2 hours took 5. What was thought to be routine was far from it. Silly, Dr. Bichell, he didn’t realize just how unique I was until he got inside. It was a hard few days after that. I was heavily sedated and there was barely a space on my body that didn’t have a probe attached or line connected. But my mom stayed by my side, and eventually I opened my eyes and joined the world.
The cardiac recovery was actually pretty quick. Within a week of the surgery they were already talking about releasing me. That is, until I got Acid reflux and started collapsing a lung. That guaranteed me two more weeks of NICU detail. Despite the location and the set-backs, we had some pretty amazing moments – like when my mom got to hold me in her arms for the first time on Mother’s Day – or when Murray Olson RT Extraordinare went above and beyond the call of duty to help my mother keep her sanity -- or when Auntie Belle found out we were here, rented a car, showed up in San Diego, and refused to leave until we did. But we were persistent in getting me released -- knowing full well I would recover better at home, and eventually we got to roll out the door. I left with a bag full of medicines, a CPAP Unit for respiratory treatments, and a ng tube down my nose (feeding tube). I wasn’t eating as well as they wanted, but that’s hardly a problem anymore! After a week of hanging around for follow-up exams, we finally got on a plane to go home – home to my dad and little-big sister – home to Kona.
It took us a while to settle into a routine. After all, I guess with medicines four times a day, respiratory treatments every 6 hours -- sometimes every 3, and eating every two hours, I was just a little high maintenance. But life found it’s “normal” for us, and the summer came and went. Then, in November, 6 months after my first surgery, I returned to San Diego for the “Glenn” – the first stage of two for the permanent fix. This time I got to take a commercial plane with my mom and sister Konane. And once again, Dad had to stay behind and keep the home fires burning.
Compared to May, November was a breeze. The surgery went really well, and mom distinctly remembers Dr. Bichell’s first words: “Your son has a strong heart.” (By the way, she brought that home with her, and that’s where Poliokekoa came from. A new name for me courtesy of Dr. Bichell, Mom, Dad, Grandma, Auntie Delma, and Auntie Bea.) I only spent 6 days in the hospital, although it wasn’t all smooth sailing. Three days after my surgery, I had a seizure. They ran three different tests (EEG, CT, and MRI) to find out why, but nothing showed up -- all clear, except for, what’s that? Evidence of an old stroke in the right brain! What???? Because no one remembers seeing me have a stroke, everyone is just assuming it was an isolated incident, probably within hours of my first surgery – while I was still unconscious. (It became obvious when I started to crawl, and I dragged my left leg behind me like a rag, but a few weeks of physical therapy, and I was crawling all over the house!)
This time we had to hang around in town a little longer. It was pretty cool for the most part. My godparents, mom, sister, and I got to go to Sea World, and my big-big sister Kayla came down from Camarillo to stay with me twice, I got to be outside every day and see the blue sky, the trees, and the sun. But just before we were supposed to go home, I got the flu and ended up in the Emergency Room. I still passed my follow-up tests, flu and all, and got to go back home for Christmas – my first Christmas.
After the holidays, I had some follow-up appointments with neurology, and three EEG’s later, there was still no evidence of the seizure. Just another unique thing about me, I guess. (Let’s hope that’s an isolated incident too!) The good thing was they stopped giving me that horrible phenobarbital. That stuff tasted like @&$#! Does it really have to taste that bad? I mean, really. With all the chemists in the world, can’t someone make a better tasting barbiturate? But I digress.
I have one more surgery to go – this November is the “Fontan” step two of two. We’ll spend another month in San Diego, and maybe this time my Dad will get to go too! But hey, that’s six months away from now.
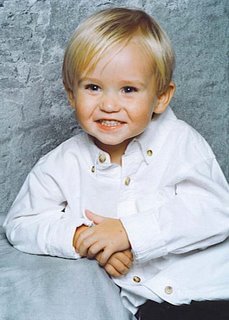
Now, it’s Spring , and I’m celebrating my first year. I am so very grateful to so many people – each one going above and beyond – each one making such a permanent, positive impact on our family.
• To Auntie Aero who helped my mom deliver me into this world on her own terms.
• To my Opa who was at the hospital before the team from Oahu, and Nana who helped Opa watch Konane while mom was in San Diego with me.
• To Auntie Gail and Dr. Lee who were there as a voice of sanity from the beginning and continue to take such wonderful care of me.
• To Grandpa and Auntie Holly who pitched in by spending time with Konane while mom was with me.
• To Grandma who helped with Konane and came to see me in San Diego.
• To my Dad for surviving a month alone with my sister Konane – not an easy task – and then another month just alone.
• To my sisters Kayla and Konane for showing me the healing touch of their love .
• To my Mom for soldiering through it all with me.
• To Dr. Bichell for having the amazing talent he does.
• To Murray Olson who took the time to reach out to my mom.
• To Auntie Belle and Uncle Eric whose undying love, support, and presence in both May and November earned them the job of Godparents.
• To Auntie Anna, Uncle Ken, and Ryder Brown – my soul mate – younger hanai brother – fellow cardiac kid and his amazing parents. For whatever reason, we are not alone in our journey.
• To everyone who said a prayer for me.
• To everyone who supported my family or wished me well.
• And finally, to God for creating such a unique individual.
I don’t know what the future holds for me yet. Will I do something amazing with my life because of this or in spite of it? Who knows, but I do know one thing, it’s been an amazing year – one filled with the most extreme highs and lows possible – and yet, this isn’t really the end of the story, is it? No, it’s just the beginning.
Mahalo nui loa for sharing this day,
and the past year,
with me.
 Little family heart story submitted by heart mom Ashlie Little.
Little family heart story submitted by heart mom Ashlie Little.